Electronic Health Records Open Brand-New Cans of Compliance Worms
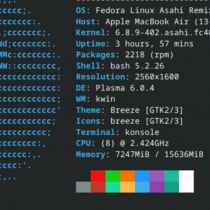
With the HITECH Act breathing down their necks, hospitals are picking up the pace of electronic health record (EHR) implementation. They face a host of familiar and emerging compliance challenges, from documentation and authentication abuses to scaling the rocky mountain of EHR “meaningful use” for purposes of collecting Medicare incentive payments and avoiding penalties.
“Electronic medical records can greatly improve documentation, but they’re not without risk,” says Cheryl Rice, vice president and chief corporate responsibility officer for Catholic Healthcare Partners, a Cincinnati-based nonprofit with 32 hospitals and many other entities. And “it’s no longer optional because of the HITECH Act.”
Hospitals and physicians receive Medicare bonuses for becoming meaningful users of certified EHR technology starting in 2011, or face payment cuts starting in 2015 if they don’t. So far, CMS defined “meaningful use” (in a Dec. 30, 2009, proposed rule) and the HHS Office of the National Coordinator set certification criteria for EHR technology in an interim final rule. As standards continue to pour forth from HHS, hospitals have to move forward the best they can, tackling sometimes-overlapping compliance demands.